Written by Chloe Hall at The Calm Gut Dietitian (www.thecalmgutdietitian.com)
Histamine intolerance (HI) can be difficult to diagnose and is often misdiagnosed due to a lack of awareness and a lack of clear diagnostic tools. Although growing, research is scarce on the most effective treatments for this condition and those with suspected HI can feel isolated and left to manage the condition on their own. In this blog, I’m going to talk about the role of histamine in the body, the causes and symptoms of histamine intolerance and what may help to reduce the symptoms of this whole-body condition.
What is histamine?
Histamine acts as a chemical messenger in our bodies and is involved in many physical processes including gastric acid secretion, inflammation and muscle contraction1,2,3,4. Histamine is produced internally by our bodies, in mast cells and other cells, and released when these cells are stimulated by a trigger, such as an illness3.
What is Histamine intolerance?
For most people histamine plays an essential role and isn’t a problem because our body has effective pathways to break internal and ingested histamine down3, 5. For others, however, for various reasons that we will discuss later in this article, there is a ‘disequilibrium of accumulated histamine and the capacity for histamine degredation’3.
Symptoms of Histamine Intolerance
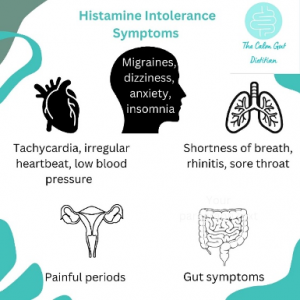
Histamine receptors can be found everywhere in the human body and HI can, therefore, cause a wide range of symptoms from dysmenorrhoea to anaphylaxis3. People with HI may find that they get different symptoms at different times, that their symptoms fluctuate or that they change over time.
Why do people experience Histamine intolerance?
HI can occur for multiple reasons. Conditions such as Mast Cell Activation Syndrome (MCAS) or mastocytosis can cause an overproduction of internal histamine3. Alternatively, in others with HI there is no overproduction in histamine but a problem with breaking it down3. Diamine Oxidase (DAO) is the primary enzyme for degrading the histamine we consume when we eat or the histamine that our gut bacteria may produce and the main reason for HI appears to be the impairment of this enzyme5,6, 7. This can happen for various reasons including gastrointestinal diseases8, medications9 or genetics3.
How do we diagnose and treat histamine intolerance?
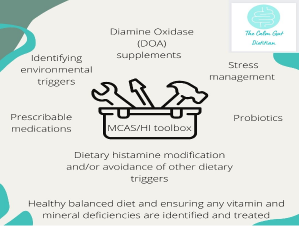
There is currently no test that we can do to accurately diagnose someone with histamine intolerance. It should be considered in anyone that presents with more than two of the above symptoms of HI5. Diagnosis currently relies on a low histamine elimination diet for 2-4 weeks with a gradual re-introduction of high histamine foods to identify a person’s tolerance level and any specific food sensitivities. This can be difficult, however, as it isn’t just food that can fill up someone’s ‘histamine bucket’ and cause it to overflow, resulting in symptoms. The low histamine diet can, also, be really restrictive, socially and nutritionally, and it is really important to do it with the support of a Dietitian who has experience in this area.

What foods are high in histamine?
There is no gold standard list of the foods high and low in histamine and many different lists can be found online. Different factors affect the histamine content of foods, even if they are widely considered low histamine, including how fresh they are and how they are stored10. Foods generally considered as high histamine foods can be found in the picture below.

Is there anything else that can help with Histamine intolerance?
There is some evidence for the use of Diamine Oxidase Enzymes (DOA), however the studies are small and the ones currently available are porcine based so may not be suitable for vegetarian’s, vegans or for religious reasons11. In addition to this, many patients with HI experience gut symptoms and may choose to trial probiotics. Some gut microbiota may produce histamine and other types can help to break it down so it is important to choose a probiotic containing the right bacterial strains6.
In conclusion
Histamine intolerance can be a very challenging condition to manage and support is crucial.
References
- Vlieg-Boerstra B.J., van der Heide S., Oude Elberink J.N.G., Kluin-Nelemans J.C., Dubois A.E.J. Mastocytosis and adverse reactions to biogenic amines and histamine-releasing foods: What is the evidence? J. Med. 2005;63:244–249.
- Russo P., Spano G., Arena M.P., Capozzi V., Fiocco D., Grieco F., Beneduce L. Are consumers aware of the risks related to biogenic amines in food. Curr Res. Technol. Edu. Top. Appl. Microbiol. Microb. Biotechnol. 2010:1087–1095.
- Maintz L., Novak N. Histamine and histamine intolerance. J. Clin. Nutr. 2007;85:1185–1196. doi: 10.1093/ajcn/85.5.1185
- Comas-Basté O., Latorre-Moratalla M.L., Bernacchia R., Veciana-Nogués M.T., Vidal-Carou M.C. New approach for the diagnosis of histamine intolerance based on the determination of histamine and methylhistamine in urine. Pharm. Biomed. Anal. 2017;145:379–385. doi: 10.1016/j.jpba.2017.06.029.
- Comas-Basté O, Sánchez-Pérez S, Veciana-Nogués MT, Latorre-Moratalla M, Vidal-Carou MDC. Histamine Intolerance: The Current State of the Art. Biomolecules. 2020 Aug 14;10(8):1181. doi: 10.3390/biom10081181.
- Pugin, B.; Barcik, W.; Westermann, P.; Heider, A.; Wawrzyniak, M.; Hellings, P.; Akdis, C.A.; O’Mahony, L. A wide diversity of bacteria from the human gut produces and degrades biogenic amines. Ecol. Healht Dis.2017, 28, 1353881.
- Smolinska, S.; Jutel, M.; Crameri, R.; O’Mahony, L. Histamine and gut mucosal immune regulation. Allergy2014, 69, 273–281.
- Schmidt WU, Sattler J, Hesterberg R , et al. Human intestinal diamine oxidase (DAO) activity in Crohn’s disease: a new marker for disease assessment? Agents Actions 1990; 30: 267–70
- Sattler J, Hesterberg R, Lorenz W, Schmidt U, Crombach M, Stahlknecht CD. Inhibition of human and canine diamine oxidase by drugs used in an intensive care unit: relevance for clinical side effects? Agents Actions 1985; 16: 91–4
- Skypala IJ, Williams M, Reeves L, Meyer R, Venter C. Sensitivity to food additives, vaso-active amines and salicylates: a review of the evidence. Clin Transl Allergy. 2015 Oct 13; 5:34 doi: 10.1186/s13601-015-0078-3
- Schnedl WJ, Schenk M, Lackner S, Enko D, Mangge H, Forster F. Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food Sci Biotechnol. 2019 May 24;28(6):1779-1784. doi: 10.1007/s10068-019-00627-3.
